- Thu. Apr 25th, 2024
Latest Post
US economic growth disappoints with 1.6 percent annualized increase, missing expectations
The U.S. economy experienced a slight slowdown during the first quarter of the year, with economic growth falling below 2 percent for the first time in over 18 months. According…
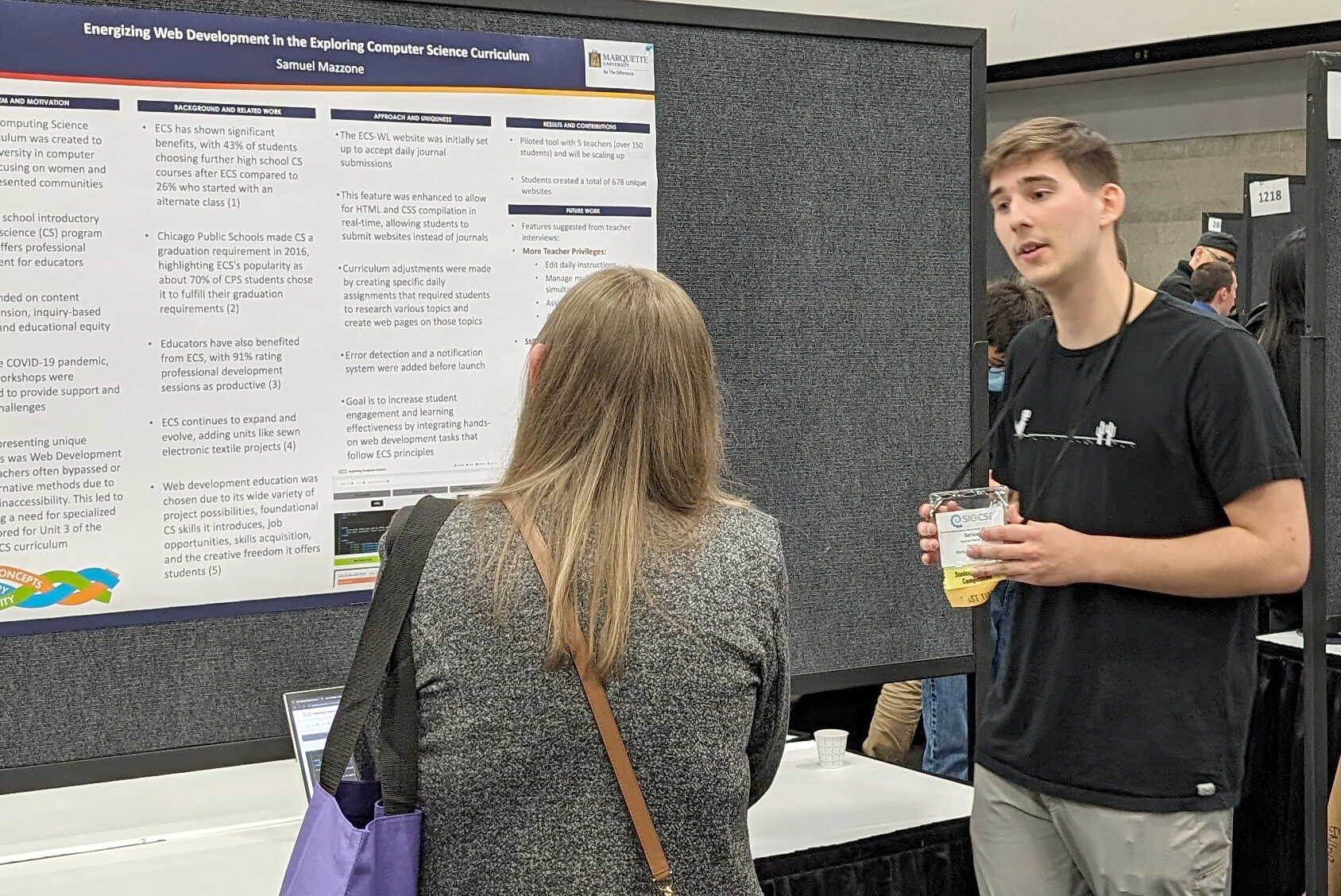
Marquette shines in computer science education at global event
Seven students from Marquette’s Department of Computer Science attended the Association for Computing Machinery SIGCSE Technical Symposium on Computer Science Education in Portland, Oregon. This conference is ACM’s leading international…
During the 2024 season, the Commanders will retire Darrell Green’s No. 28
During the 2024 season, the Washington Commanders franchise legend Darrell Green will have his No. 24 retired, as announced by the team on Thursday. Green, who spent all 20 seasons…
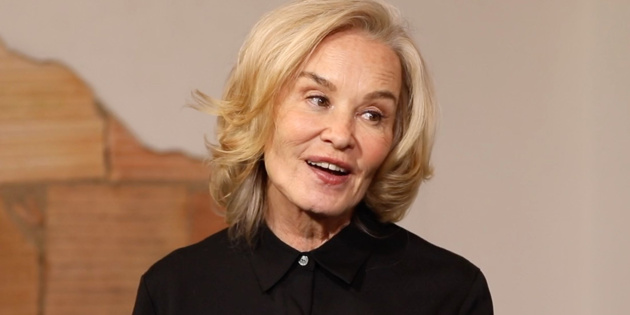
Jessica Lange is thrilled to unveil the world premiere of Mother Play on Broadway – a new venture for the acclaimed actress
Jessica Lange has had a successful Broadway career, taking on classic American stage roles one after the other. From her debut in 1992 as Blanche DuBois to her Tony Award-winning…
Growth Stalls as U.S. Economy Expands by 1.6% in Last Quarter
The U.S. economy saw a slowdown in growth at the beginning of 2022, marking its slowest pace since the second quarter of 2022. Despite this slowdown, there are still few…
Former Federal Trade Commission and White House alum joins anti-monopoly watchdog: Lobbying World
Elizabeth Wilkins, who previously worked at the Federal Trade Commission as the chief of staff to the chair and director of the Office of Policy Planning, is joining the American…
From civil twilight to nautical twilight: Exploring the science of sunrises and sunsets
Sunrise and sunset are two of the most stunning moments of the day, where the sky is painted with shades of pink and orange. However, what happens before and after…
US Economy Grows at Slowest Pace in 2 Years in Q1: GDP at 6.1% Misses Estimates Due to Sharp Uptick in Core Inflation
The US economy experienced its slowest growth in two years last quarter, with consumer and government spending cooling down alongside a significant increase in inflation. The US gross domestic product…
GlaxoSmithKline files lawsuit against Pfizer and BioNTech for Covid-19 vaccine technology
GlaxoSmithKline filed a lawsuit against Pfizer and BioNTech in Delaware federal court, alleging that the companies’ COVID-19 vaccines, Comirnaty, infringe on GSK’s patents related to messenger RNA (mRNA) technology. GSK…
Yellen: Economy is Strong, Inflation Expected to Decrease
During an interview with Reuters, Treasury Secretary Janet Yellen expressed her optimism about the performance of the U.S. economy, stating that it is continuing to do very well. Despite data…